The Premise
Modern dentistry has evolved beyond simple fillings and extractions. Today, patients often undergo comprehensive smile makeovers that involve a “mixed media” approach: titanium implants to replace missing roots, porcelain veneers to perfect aesthetics, and orthodontic hardware to align the architecture. While these advancements create stunning visual results and restore function, they also introduce a new level of biological complexity. A mouth containing natural teeth, ceramic restorations, and implant fixtures requires a specialized, high-performance maintenance routine. For patients in Caledonia, understanding the unique hygiene requirements of these materials is not just about cleanliness—it is about protecting a significant investment and ensuring the longevity of the restoration.
Introduction
The journey to a perfect smile is often a marathon, not a sprint. It involves meticulous planning, surgical intervention, and months or years of orthodontic movement. However, once the braces are removed and the implants are loaded, the journey is not over; it shifts into a critical maintenance phase.
The oral environment is hostile. It is constantly subjected to bacteria, acid, temperature fluctuations, and mechanical force. Natural teeth have biological defences against these aggressors, such as the periodontal ligament and gingival fluid flow. Artificial restorations, however, lack these self-defence mechanisms. A dental implant, for instance, connects to the bone and gum differently than a natural tooth, making it more susceptible to a specific type of inflammation if plaque is not managed aggressively. Similarly, veneers create microscopic margins where bacteria can hide, and braces create physical barriers that disrupt the natural cleansing action of saliva.
When a patient has a combination of these treatments—such as an adult using clear aligners while stabilizing a dental implant—the hygiene protocol must be customized. Generic advice like “brush and floss” is no longer sufficient. This article outlines a specialized care strategy, detailing the tools, techniques, and professional insights required to maintain a healthy mouth amidst complex dental work.
1. The Biological Difference: Mucosal Seal vs. Periodontal Attachment
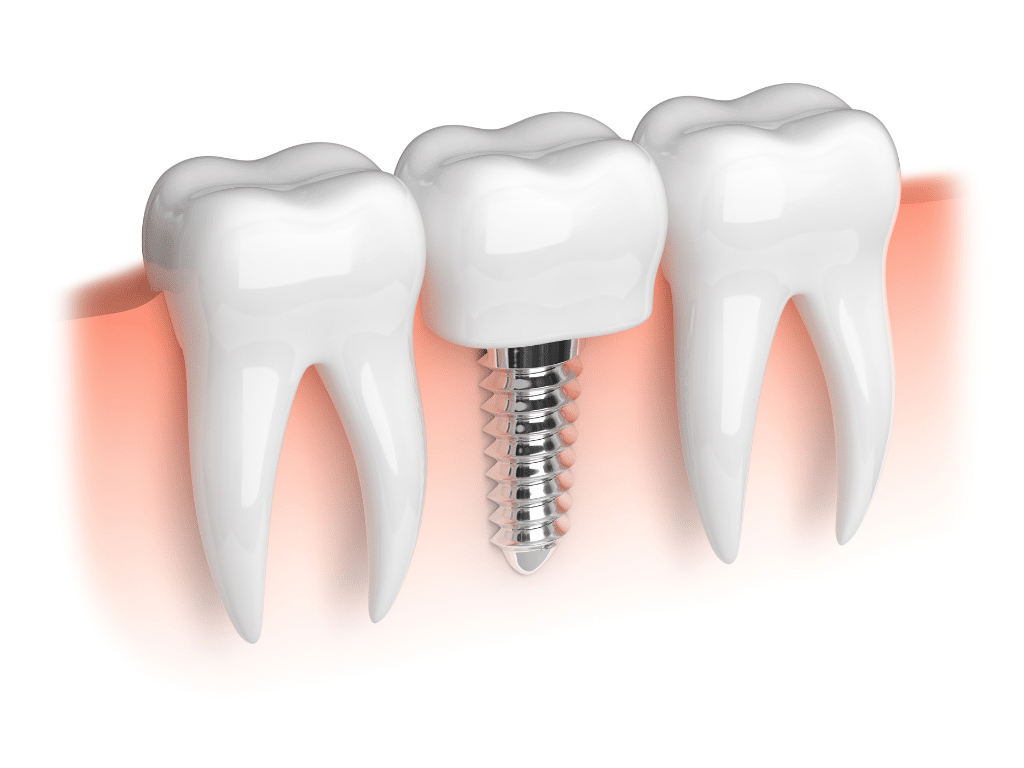
Descriptive Paragraph To understand why specialized hygiene is necessary, one must first understand the anatomical differences between a natural tooth and a dental implant. A natural tooth is attached to the jawbone by the periodontal ligament (PDL), a shock-absorbing tissue that also supplies blood and immune cells to the area. This helps the tooth fight off minor bacterial invasions. A dental implant, however, lacks a PDL. It relies on osseointegration (direct bone-to-metal contact) and a “mucosal seal” of gum tissue around the neck of the implant. This seal is weaker and less vascular than the attachment around a natural tooth, creating a path of least resistance for bacteria.
Detailed Information
- The Defence Deficit: Because implants lack the blood supply provided by the PDL, the immune response to plaque accumulation is slower and less effective. This means that inflammation can spread into the bone much faster around an implant than around a natural tooth.
- Connective Tissue Orientation: The collagen fibers in the gums attach to a natural tooth perpendicularly, acting like a zipper that seals out bacteria. Around an implant, these fibers run parallel to the surface, resembling a rubber band. This “rubber band” is easier for bacteria to push past, making meticulous plaque control mandatory.
- Tactile Sensitivity: Natural teeth have nerves that signal pressure or pain (proprioception). Implants do not. A patient might not feel the early warning signs of infection or aggressive brushing damage around an implant until significant bone loss has occurred.
- Vulnerability Phase: If a patient is undergoing orthodontic treatment with a temporary crown on an implant, the gum tissue is constantly remodeling. This transient state creates pockets where food debris can easily become trapped, requiring hyper-vigilance during the braces phase.
2. Navigating Orthodontic Hardware: Brackets, Wires, and Aligners
Descriptive Paragraph When braces or aligners are introduced to a mouth that also contains veneers or implants, the surface area for bacterial retention increases exponentially. Orthodontic appliances are notoriously efficient plaque traps. In a standard mouth, plaque accumulates at the gum line. In an orthodontic mouth, plaque accumulates around every bracket, under every wire, and inside every aligner attachment. If this plaque is left undisturbed, it produces acid that can etch natural enamel (white spot lesions) and inflame the tissues supporting the implants and veneers.
Detailed Information
- The pH Drop: Orthodontic hardware restricts saliva flow to certain areas of the tooth. Saliva is the mouth’s natural buffer against acid. Without it washing over the tooth surface, the pH drops, and demineralization begins. For patients with veneers, this can lead to decay at the margin where the veneer meets the natural tooth structure.
- Aligner Hygiene: Patients using clear aligners often trap acid against their teeth. If a patient drinks a sugary beverage or coffee and puts their aligners back in without brushing, the liquid is held against the enamel and the implant crown for hours. This acts like an acid bath, accelerating decay and staining.
- Interproximal Challenges: Wires prevent standard flossing. Patients must use threaders or specialized orthodontic floss (like Superfloss) that has a stiff end to navigate between the teeth and the wire. Failure to do this results in hypertrophic (swollen) gums that can grow over the brackets.
- Water Flosser Utility: For patients with manual dexterity issues, or those with extensive hardware, a water flosser is indispensable. It uses a pressurized stream of water to blast debris out from behind wires and around implant abutments where string floss cannot reach.
3. Peri-Implantitis: The Silent Threat
Descriptive Paragraph The equivalent of gum disease (periodontitis) for an implant is called peri-implantitis. It is the leading cause of late-stage implant failure. It begins as peri-implant mucositis—a reversible inflammation of the soft tissue—but if left untreated, it progresses to bone loss. Unlike natural teeth, which may become loose when they lose bone, implants often remain rock solid until the very end, masking the severity of the infection. Preventing this condition is the primary goal of hygiene for implant patients.
Detailed Information
- Early Warning Signs: Bleeding upon probing or flossing is the cardinal sign of mucositis. Patients often stop flossing when they see blood, thinking they are injuring the gum. In reality, they need to clean more gently and thoroughly to remove the bacteria causing the bleeding.
- The “Rough” Surface: Dental implants often have a roughened surface texture to encourage bone growth. If gum recession occurs and this rough surface is exposed to the oral cavity, it becomes a magnet for plaque and calculus (tartar) that is nearly impossible to clean with a toothbrush alone.
- Cement Sepsis: Sometimes, excess cement used to glue the crown onto the implant can get trapped under the gum line. This acts as a foreign body, causing chronic inflammation. Regular X-rays during hygiene visits are essential to detect these sub-gingival irritants.
- Progression Speed: Studies show that bone loss around an infected implant can progress significantly faster than around a natural tooth. This makes the “wait and see” approach dangerous. Immediate intervention with deep cleaning or laser therapy is required at the first sign of trouble.
4. Veneer Maintenance: Protecting the Margins
Descriptive Paragraph Porcelain veneers are incredibly durable and resistant to staining, but they are not invincible. The weak link in a veneered tooth is the margin—the microscopic line where the porcelain ends and the natural tooth structure begins. If the gums recede due to aggressive brushing or gum disease, this margin becomes exposed. Not only is this aesthetically displeasing (often showing a yellow line of root structure), but it exposes the tooth to decay. Hygiene for veneers focuses on maintaining the position of the gum line and keeping the margins sealed.
Detailed Information
- Non-Abrasive Pastes: Many “whitening” toothpastes contain abrasive particles (like silica) designed to scrub stains off enamel. These abrasives can scratch the glaze on porcelain veneers, making them dull and more prone to attracting stain over time. Patients should use non-abrasive gels or pastes specifically designed for cosmetic dentistry.
- Alcohol-Free Mouthwash: High-alcohol mouthwashes can soften the bonding composite resin that holds the veneer to the tooth. Over years of use, this can lead to micro-leakage at the margins, causing sensitivity and eventual debonding.
- Flossing Technique: When flossing a veneer, one must be careful not to “snap” the floss out. Instead, pull the floss through to the side. Snapping the floss upward can catch on the ledge of the veneer and, in rare cases, dislodge it.
- Bite Guards: Patients with veneers are often prescribed a night guard. This is a hygiene device as much as a protective one. It prevents bruxism (grinding) forces from cracking the porcelain, which would create rough surfaces that harbor bacteria.
5. Specialized Tools for the “Hybrid” Mouth
Descriptive Paragraph A standard flat-trimmed toothbrush is rarely sufficient for a mouth containing implants, braces, and veneers. The topography of the mouth is too complex. Implants often have a narrower diameter near the gum line than the crown they support, creating an undercut or “mushroom” shape that a regular brush misses. Effective hygiene requires a toolkit of specialized instruments designed to navigate these contours without damaging the hardware.
Detailed Information
- Interdental Brushes: These are small, pine-tree-shaped brushes that fit between teeth. They are superior to floss for cleaning the concave surfaces of implant roots and the spaces opened up by orthodontics. They must be plastic-coated wire; exposed metal wire can scratch the titanium implant surface.
- End-Tuft Brushes: This is a toothbrush with a very small, circular head. It is perfect for cleaning around the brackets of braces, the back of the very last molar, and the gum line of implants where a regular brush head is too bulky to reach.
- Sulcus Brushes: These brushes have two rows of soft bristles and are designed specifically to clean the gingival sulcus (the pocket between the tooth and gum). They are essential for preventing mucositis around implants.
- Rubber Tip Stimulators: While an older tool, the rubber tip is excellent for massaging the gum tissue between teeth (the papilla). This increases blood flow and helps reshape the gum tissue after orthodontic movement or implant surgery.
6. Professional Hygiene Visits: The Scaling Protocol
Descriptive Paragraph The hygiene appointment for a patient with implants and veneers looks very different from a standard cleaning. Dental hygienists in Caledonia must use specific protocols to avoid damaging the restorations. Standard stainless steel scalers, which are used to scrape tartar off natural teeth, can gouge the surface of a titanium implant. These scratches create a rough surface where bacteria can thrive, increasing the risk of infection. Therefore, the “tools of the trade” must change.
Detailed Information
- Resin and Carbon Fiber Scalers: Hygienists use instruments made of medical-grade plastic, resin, or carbon fiber to clean implants. These are softer than titanium and will not scratch the surface, yet are strong enough to remove soft plaque and calculus.
- Ultrasonic Considerations: Standard ultrasonic tips (the water-vibrating tools) can also damage porcelain and titanium. Specialized PEEK (plastic) tips are used on ultrasonic units to safely vibrate deposits off implants and veneers.
- Air Polishers: Modern hygiene often involves air-flow therapy, which uses a mix of water, air, and fine powder (like glycine or erythritol) to blast away biofilm. This is gentle on soft tissues and safe for implant surfaces, providing a superior clean compared to traditional rubber cup polishing.
- Fluoride Varnish: While titanium doesn’t need fluoride, the natural teeth next to it do. Neutral sodium fluoride is preferred over acidulated phosphate fluoride (APF), as the acid in APF can etch the surface of porcelain veneers and corrode the oxide layer on titanium implants.
7. The Impact of Diet on Multi-Material Smiles
Descriptive Paragraph Hygiene is not just about cleaning; it is about controlling the input. Diet plays a massive role in the longevity of restorative work. When a patient has braces, implants, and veneers, the mechanical and chemical impact of food changes. Foods that are safe for natural teeth might be hazardous for veneers (due to leverage forces) or braces (due to stickiness). Furthermore, a high-sugar diet feeds the specific bacteria that cause peri-implantitis.
Detailed Information
- The “Sticky” Factor: Caramel, taffy, and gum are the enemies of orthodontics. They can pull wires out of brackets. For implant patients, sticky foods can create a suction force that, while unlikely to pull out an integrated implant, can loosen the screw retaining the crown.
- Hard Foods and Leverage: Biting directly into an apple or corn on the cob puts sheer force on the front teeth. Natural teeth have ligaments to absorb this; implants do not. This force is transferred directly to the bone or the porcelain veneer, leading to fractures. Patients are advised to cut hard foods into pieces.
- Staining Agents: Porcelain veneers are stain-resistant, but the bonding cement at the edges is not. Heavy consumption of turmeric, red wine, or coffee can lead to “framing,” where the edge of the veneer turns brown. Sipping through a straw and rinsing with water after meals helps mitigate this.
- Anti-Inflammatory Diet: Chronic inflammation is the enemy of implants. A diet rich in antioxidants, Omega-3 fatty acids, and low in processed sugars supports the immune system in maintaining the seal around the implant.
8. Managing Hygiene During the “Coordination” Phase
Descriptive Paragraph The most difficult hygiene period is often during the active treatment phase, where implants are placed while braces are still on. In these scenarios, the patient might have a surgical site with sutures, a healing abutment (a metal cap poking through the gum), or a temporary pontic suspended from an archwire. Cleaning around a fresh surgical site that is obstructed by orthodontic wires requires extreme delicacy and specific techniques to prevent infection without disrupting the healing process.
Detailed Information
- Chlorhexidine Rinses: Immediately after implant surgery, mechanical brushing might be too painful or risky. Dentists often prescribe a Chlorhexidine gluconate mouthwash. This is a powerful antiseptic that chemically controls plaque when brushing is impossible. However, it can stain teeth brown if used too long, so it is strictly for the short-term healing phase.
- Surgical Site Avoidance: If an implant has just been placed, the patient must not use a water flosser on that specific area for several weeks, as the pressure can disturb the blood clot and bone graft.
- Cleaning Under Pontics: If a fake tooth is attached to the braces wire to hide a gap, it creates a “roof” over the gum. Patients must use a floss threader to pass floss under this pontic daily to massage the gum, otherwise, the tissue will become boggy and bleed during the final impression stage.
- TAD Hygiene: If Temporary Anchorage Devices (mini-implants) are used for orthodontics, they must be brushed gently. Because they penetrate the gum, they can easily get infected and become loose. A cotton swab dipped in mouthwash is often used to clean the head of the TAD.
9. Chemical Adjuncts: Beyond Toothpaste
Descriptive Paragraph For the high-risk patient with complex restoration, mechanical cleaning (brushing/flossing) is sometimes not enough to lower the bacterial load. Chemical adjuncts—mouthwashes, gels, and varnishes—become necessary tools in the hygiene arsenal. However, the chemistry matters. The goal is to reduce bacteria without damaging the surface properties of the titanium or porcelain.
Detailed Information
- Oxidizing Agents: Mouthwashes containing hydrogen peroxide can be beneficial for whitening natural teeth, but prolonged use can alter the surface of titanium. Patients should consult their dentist before adopting a daily whitening rinse.
- Essential Oils vs. CPC: Mouthrinses with essential oils (like Listerine) or Cetylpyridinium chloride (CPC) are effective at penetrating the biofilm (slime layer) that bacteria build on implants. These are generally safe for daily use to reduce the overall bacterial count in the mouth.
- Probiotics: Oral probiotics are an emerging field. They involve introducing beneficial bacteria (like Streptococcus salivarius) to the mouth to outcompete the harmful pathogens that cause peri-implantitis and decay. This is particularly useful for patients who are prone to infections.
- Remineralization Pastes: Products containing calcium phosphate (like MI Paste) can help strengthen the enamel around orthodontic brackets, preventing the “white halo” scars that often appear after braces are removed.
10. The Lifetime Commitment: Retention and Recalls
Descriptive Paragraph The removal of braces marks the beginning of the retention phase. For patients with implants and veneers, retention is doubly important. If teeth shift, they can create traumatic bite forces on the rigid implant or veneer, leading to fracture or bone loss. Therefore, hygiene also encompasses the care and cleaning of retainers (Hawley, Essix, or bonded fixed retainers). A dirty retainer is a petri dish that re-introduces bacteria to the clean mouth every night.
Detailed Information
- Bonded Retainers: A permanent wire glued behind the front teeth is excellent for stability but is a hygiene nightmare. It requires the daily use of floss threaders. Calculus builds up heavily around these wires; if this calculus pushes on the gum around a nearby implant, it can trigger peri-implantitis.
- Retainer Cleaning: Retainers should never be cleaned with hot water (which warps them) or toothpaste (which scratches them, making them cloudy and retentive to bacteria). They should be cleaned with cool water and specialized retainer tablets or mild soap.
- Night Guard Hygiene: Hard acrylic night guards can accumulate calcium deposits. They need to be scrubbed daily and brought to dental appointments so the hygienist can put them in a professional ultrasonic cleaner.
- Customized Recall Intervals: The standard 6-month checkup is often inadequate for complex cases. Patients with implants and a history of gum disease often require a 3-month or 4-month interval. This frequency disrupts the bacterial life cycle before it can organize into a destructive colony.
Conclusion
A smile reconstructed with dental implants, veneers, and orthodontics is a marvel of modern medical engineering. It restores confidence, function, and aesthetics. However, the biological reality is that this “bionic” smile requires a level of care that exceeds that of a natural set of teeth. The mix of materials—titanium, porcelain, resin, and enamel—creates a unique environment that reacts differently to bacteria and physical force.
For residents of Caledonia, embracing specialized hygiene habits is the insurance policy on this investment. It requires the right tools, from water flossers to interdental brushes; the right chemistry, from non-abrasive pastes to pH-neutral fluorides; and the right professional partnership. By understanding the vulnerabilities of implants and the plaque-trapping nature of orthodontics, patients can take proactive steps to prevent infection and failure. With dedicated care, a complex smile makeover can remain healthy, functional, and beautiful for a lifetime.
Protect Your Investment
Expert Care for Complex Smiles.
Your smile is a masterpiece of engineering. Don’t let improper maintenance compromise your results. Whether you are navigating life with braces, caring for new implants, or maintaining veneers, the team at Dentistry at the Plex is here to guide your specialized hygiene journey.
- Name: Dentistry AT The Plex
- Address: 370 Argyle St S, Caledonia, ON N3W 2N2
- Phone: 289.960.0730
- Email: Send an email to [email protected]
- Website: Visit their website at www.dentistryattheplex.com.
Protecting the Investment Behind Your Smile